GLC4HSR concludes Annual Conclave 2024; advances dialogue on resilient health systems
Updates ▪ Mar 13, 2024
The Conclave of the Global Learning Collaborative for Health Systems Resilience (GLCHSR), held it 2nd Annual on March 11th and 12th, bringing together over 500 participants, both virtually and in-person. The event featured 60+ speakers from over 15 countries, offering insights into various aspects of resilient health systems.
The Conclave was a testament to collective knowledge and collaboration. It covered topics ranging from redefined models for health systems assessment to discussions on future-ready surveillance systems, addressing climate change impacts, emphasizing community engagement, and advocating for gender equity in health systems. Participants engaged in meaningful dialogues around enhancing healthcare provision, ensuring supply chain resilience, exploring innovative financing mechanisms, and embracing digital transformation. This collective effort reflects the spirit of the GLC4HSR and a common vision of creating a healthier and more resilient future.
ACCESS Health and GLC4HSR thank the Annual Conclave knowledge partners: Health Systems Global and Duke-NUS Centre of Regulatory Excellence; Co-hosts: Asia-Pacific Cardiovascular Disease Alliance and Women in Global Health Singapore; and session sponsor: US Pharmacopeia. Their support and collaboration were instrumental in making this event a success, enriching discussions, and driving meaningful outcomes. We also thank all the speakers for sharing their expertise and insights, contributing to the dialogue, and inspiring collective action towards building resilient health systems.
Follow us on LinkedIn and watch the session recordings on our YouTube channel.
Inaugural session by Dr. Sohel Saikat:
- Dr. Saikat highlighted WHO's initiatives and GLC4HSR's intentional actions toward global Health Systems Strengthening, emphasizing resilience measurement tools and core system functions.
- Outlined WHO's toolkit for resilience measurement and operationalization steps, including prioritization, baseline identification, integrated planning, institutionalization, and progress monitoring.
- Discussed WHO's recovery planning guide emphasizing integrated approaches and learning from crisis for resilient healthcare systems.
- Emphasized the importance of real-time data, crisis learning, and integrating healthcare for global resilience.
- Highlighted the role of assessment indicators in defining health system resilience and continuous improvement.
Health Systems Resilience Assessment: India and UAE Insights:
- Proposed strategies for knowledge sharing and best practice adoption between countries, facilitating mutual learning and enhancing global health system resilience.
- Stressed the importance of community resilience and health literacy for sustainable engagement and resilient tool adaptation.
- Emphasized identifying and addressing data gaps through documentation and integrating quantitative and qualitative data into public health systems.
- Highlighted the essential role of collaboration across governmental levels for effective integration of health system indicators.
- Advocated for private sector inclusion in dialogues, especially in addressing profitability gaps and enhancing national resilience through policy integration.
- Emphasized the immediate collection of real-time data and the need for a comprehensive approach involving both society and government for effective challenges addressing.
- Highlighted the importance of adaptable frameworks that can withstand disruptive forces, ensuring resilience to unforeseen challenges and disruptions.
Roadmap Towards Building Better Surveillance-Alert-Response-Systems:
- Advocated for cross-sector collaboration to develop surveillance systems and translate data into policies.
- Highlighted leveraging media for alerts and combating misinformation through standardized reporting.
- Prioritized addressing critical questions in underserved areas for essential services improvement.
- Emphasized maintaining consistent infrastructure for collaboration, particularly in research and critical service delivery.
- Stressed economic viability for scalable initiatives and financial sustainability in surveillance systems.
Adapting to Climate Change: Operationalizing Health System Resilience:
- Stressed planning and pre-implementation phases' importance, quick wins, and community trust building.
- Discussed resilient health infrastructure aspects, including emergency departments and systemic resilience.
- Emphasized environmental impact assessments and decarbonizing processes for climate change mitigation.
- Advocated synthesizing lessons learned into cohesive policy frameworks for future resilience policies.
- Recognized NGOs' role, community engagement, and sustainability shift towards community-driven actions.
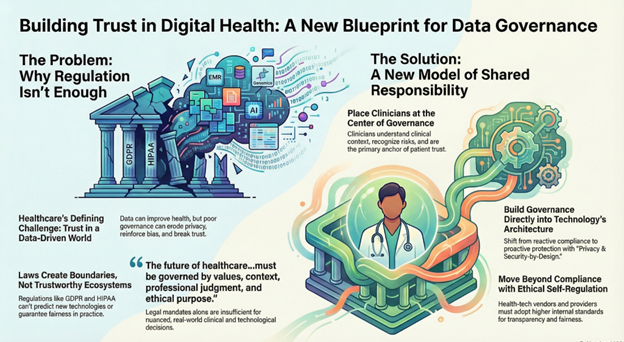
Charting Pathways for Equitable and Resilient Digital Health Ecosystems
- Enhance institutional capabilities at various levels, including provincial, city, and district levels, for effective health data collection.
- Highlight the significance of health data governance within digital transformation strategies to foster collaboration across sectors.
- Advocate for balancing innovation and regulation while promoting collaboration to accelerate desired outcomes in digital health initiatives.
- Acknowledge the challenges in implementing digital transformation blueprints and emphasize the need to translate plans into actionable strategies.
- Stress the importance of addressing the gap between AI potential and backend system capabilities for successful integration into healthcare systems.
Exploring Community Engagement: Unpacking Purpose, Policy, People, and Planet:
- Recognize the crucial role of NGOs in public health interventions, particularly in areas like family planning and immunization, with significant impacts.
- Emphasize the importance of providing NGOs with space, freedom, and adequate
- Highlight NGOs' excellence in social mobilization, often prompting government action on pressing health issues.
- Advocate for engaging the community in public health programs to foster a sense of ownership and sustainability, transitioning from NGO-led initiatives to community-driven actions.
Day 2 Opening Address by Dr. Nima Asghari-Jirandeh:
- Emphasized inclusivity and gender equity in healthcare policies and practices.
- Advocated for sustainable financing strategies for long-term healthcare resilience.
- Highlighted the importance of integrating digitalization and regulatory frameworks for enhanced health system resilience.
- Addressed the impact of policy beyond traditional health sectors, focusing on climate change readiness and primary healthcare transition.
- Stressed the need for collaborative efforts in integrating digital technologies into healthcare systems.
Applying a multi-pronged approach for supply chain resilience
- Identified five key elements essential for building and sustaining a strong supply chain in healthcare.
- Emphasized the significance of supply chain transparency, standardized data, and advanced manufacturing technologies.
- Discussed challenges such as fragmentation and lack of standardization downstream in healthcare supply chains.
- Highlighted the role of regulators, manufacturers, and healthcare providers in ensuring the affordability, safety, and quality of medications.
- Panel discussions focused on examining vulnerabilities, implementing quality systems, and addressing global supply chain issues.
Utilizing innovative financing to strengthen resilient health systems
- Advocated for bridging gaps between climate-focused investments and healthcare infrastructure.
- Proposed market mechanisms, matching funds, and innovative financing models for sustainable health system development.
- Emphasized the importance of transparency, flexibility, and taxation in healthcare financing strategies.
- Discussed broader regional perspectives on healthcare financing, aging, and retirement costs.
- Panel discussions explored the role of private sector funding, taxation, and innovative financing mechanisms in achieving sustainable health systems.
Special Session on CVD care by the APAC CVD Alliance
- Enhanced sharing of shared experiences among healthcare providers can significantly reduce unnecessary appointments.
- Investing in community empowerment and engagement, particularly in health literacy and self-help groups, is vital for both primary and secondary prevention efforts.
- There is curently an underutilization of pharmacy services for ensuring continuity of care and patient adherence, both within and outside hospital settings. Overcoming clinical inertia and facilitating multidisciplinary collaboration is essential for initiatives like cardiac rehabilitation clinics.
- Effective governance at the system level involves three crucial perspectives: the community's role, provider system innovations, particularly in processes, and the payer's perspective in disease control strategies.
Ensuring Preparedness and Building Resilience of Healthcare Provision During Public Health Emergencies
- Highlighted the critical elements of primary healthcare, community empowerment, and multisectoral action in health system resilience.
- Emphasized the need for proactive measures, political commitment, and continuous learning in healthcare provision during emergencies.
- Advocated for resource mobilization, telemedicine, and real-time monitoring for effective emergency response.
- Discussed the role of digital technologies, data sharing, and community-based programs in healthcare preparedness.
Equity in Healthcare Careers for Health Systems Resilience:
- Addressed gender biases and barriers in healthcare careers, advocating for equality, inclusion, and support for women in leadership roles.
- Advocated for gender-neutral practices, policy support, mindset changes, and community empowerment to promote gender equity and resilience in healthcare systems.
- Highlighted the importance of establishing policies, structures, and governance that support gender equality for greater gender equity in healthcare careers.
- Stressed the significance of societal mindset changes, recognizing challenges faced by women leaders, and efforts to uplift and train women into leadership roles.
- Advocated for addressing gender biases to foster inclusivity, community resilience, and empowerment in healthcare settings.